Surgical techniques
Anatomy of the distal femur
On the lateral view the shaft is aligned with the anterior half of the lateral condyle.
The distal femur is trapezoidal
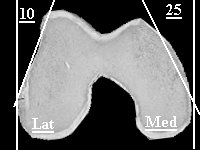


- Anterior surface slopes downward from lateral to medial,
- Lateral wall inclines 10 degrees
- Medial wall inclines 25 degrees.
knee joint is parallel to the ground
anatomic axis (the angle between the shaft of the femur and the knee joint) has a valgus angulation of 9 degrees (range, 7 to 11 degrees)
Approaches
Radiolucent table, small sand bag under ipsilateral hip, free drape leg. If nailing use triangle/ bolster under knee to flex slightly(30-40 degrees), allows easier entry.
Lateral approach most commonly used exposure. Suitable for all fractures except with fracture limited to medial femoral condyle.
- Lateral skin incision centred over lateral condyle across joint then curve gently anterior to end just lateral to tibial tuberosity
- Through iliotibial band, through joint capsule and synovium exposing lateral femoral condyle (inferior geniculate art.). Don't cut lateral meniscus.
- Elevate Vastus lateralis from intermuscular septum, ligating perforators. Exposing lateral femoral condyle.
More access
- Add tibial tuberosity osteotomy ( pre drill hole). Detach fat pad from tibia and reflect Quadriceps mechanism.
- Alternative - Z-shaped tenotomy of the infrapatellar tendon. If used protect with wire band 12 weeks
Anterior approach
- Anterolateral skin incision
- Lateral parapatellar arthrotomy
- Vastus lateralis is elevated off the lateral femoral cortex. Anterior skin incision allows better visualisation of medial femoral condyle.
Medial Approach (fracture limited to medial condyle, severly comminuted needing double plating)
- Straight medial skin incision over the thigh distally over the medial condyle anterior to the adductor tubercle.
- Incise deep fascia in line with the skin incision,
- Elevate vastus medialis from the adductor magnus (medial geniculate artery)
- Medial patellar retinaculum, joint capsule, and synovium. Stay anterior to medial collateral ligament and avoid medial meniscus.
- Beware femoral art. and V.
Anterolateral approach ( complex intra articular fractures)
- As for TKR midline and medial parapatella, sublux patella laterally.
- Offers excellent exposure of articular surface.
Implants
For all first step is exposure and reconstruction of articular surface with lag screws if needed. Placing lag screws away from entry points of individual implants.
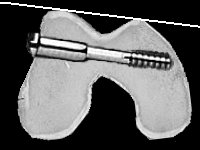
95 Degree Blade plate
Mark site of entry of blade plate
 |
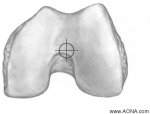
1.5-2 cm from distal articular surface centered on a point in the middle of the anterior 1/2 of the lateral condyle. |
Mark trajectory
 |
Frontalplane - parallel to the joint surface. Transverse plane - between the patellar groove anteriorly and the intercondylar notch posteriorly. Place K wire along the distal articular surface, and another across the anterior surface of the femur, over the patellar groove. Insert third K-wire into the lateral femoral condyle distal to the marked blade entry site Parallel to the distal K-wire in the frontal plane and parallel to the anterior K-wire in the transverse plane. Check position of third k wire on image intensifier and use third wire to guide central drill hole. |
Finally control the rotational position of the blade in the coronal plane (i.e., flexion and extension) should be such that the plate will align with the femoral shaft. Think of this when drilling top and bottom of 3 drill holes. Then join 3 holes with seating chisel.
Remember the trapezoidal cross section of the femur, therefore measure the most anterior distance in the channel. Use of radiographs or the depth of the posterior end of the slot for the determination of blade length will result in medial protrusion of the blade.Ensure 8 cortices proximal fixation to the shaft
NB A blade not parallel to the joint will induce a varus or valgus deformity
Because of the trapezoidal shape of the distal femur, a posterior blade entry point will result in a medialization of the distal segment, along with increasing the risk of notch penetration.
A mal-rotation of the blade will result in flexion or extension deformity
Dynamic Condylar Screw
The plate-barrel (screw) angle is 95 degrees, as in the blade plate.
Once the screw is placed, flexion and extension can still be adjusted, unlike the blade plate.
It does not afford good rotational control unless a screw from the side plate engages the distal fragment viz implications for distal fractures.
 |
Insert guide wire as for
centre of blade plate, slightly more proximal (2 cm from the joint surface
at the junction of the anterior 1/3rd and
posterior 2/3rds of the longest AP dimension of the
lateral femoral condyle or in the middle of the anterior
half of the lateral femoral condyle) Trajectory as for blade plate. Advance guide wire to medial cortex (remember trapezoidal shape), measure depth. Ream and place screw 5 to10 mm shorter than measured to avoid soft tissue irritation
Insert screw as for DHS remember alignment of handle to align side plate. Insert at
least one screw from side plate into distal fragment to control flexion/
extension |
The above can be done by a mini invasive technique as described by Russell using a femoral distractor placed on the lateral side of the leg with two 5-mm Schanz pins.
Retrograde Locked Intramedullary Nails (including supracondylar
nail)
Medial parapatella approach or minimally invasive split patella tendon.
 |
Entry point in line with intramedullary canal, centre intercondylar notch anterior to origin of PCL on femur Locking configuration depends on make of nail. At least two distal screws to control flexion and extension. Reamed or unreamed If intercodylar split ream opening to avoid seperating condyles.
|
Russell, George V. Jr. MD. Smith, Douglas G. MD. Minimally Invasive Treatment of Distal Femur Fractures: Report of a Technique. Journal of Trauma-Injury Infection & Critical Care. 47(4):799, October 1999